What’s the Buzz
The Bee Healthy Blog
What Are The Stages of Interstitial Lung Disease?

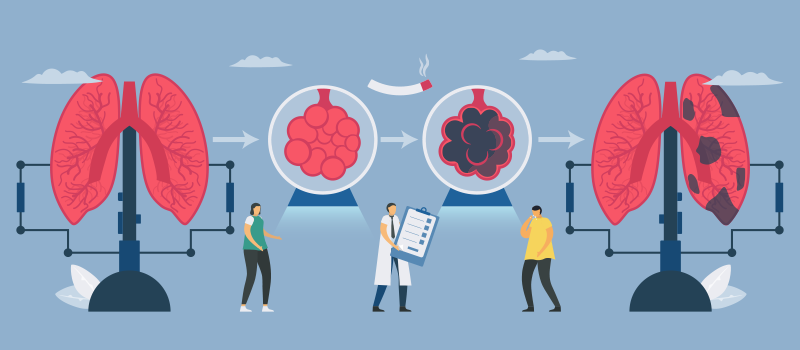
Interstitial lung disease (ILD) is a collective term for more than 200 potentially life-threatening illnesses that cause inflammation and fibrosis (scarring) of lung tissue. They are chronic progressive conditions that cause worsening fibrosis over time. As a person develops more lung scarring, it becomes harder for them to breathe and get oxygen into their bloodstream. Please continue reading to learn more about interstitial lung diseases, including the symptoms, causes, risk factors, stages, diagnosis, and treatment options.
What are interstitial lung diseases?
Interstitial lung diseases are conditions of the lower respiratory tract in which the lung tissue between the alveoli (air sacs) and lung capillaries (small blood vessels) is damaged by inflammation and fibrosis (scarring). This causes irreversible lung damage and affects the lung tissue’s ability to move air and oxygenate the blood. Another name for ILD is diffuse parenchymal lung disease (DPLD).
What causes interstitial lung disease?
Smoking and exposure to environmental or occupational pollutants are major contributing factors for interstitial lung disease. However, sometimes the condition is idiopathic (the exact cause is unknown), for example, idiopathic interstitial pneumonia. Doctors believe interstitial lung disease occurs when injuries to the lung tissue trigger an abnormal healing response. As a result, lung tissue thickens, and scar tissue forms.
Is the condition called pulmonary fibrosis the same as interstitial lung disease?
As mentioned, there are more than 200 types of interstitial lung disease. Idiopathic pulmonary fibrosis (IPF) is a common type of ILD. Therefore, while idiopathic pulmonary fibrosis (IPF) is an interstitial lung disease, not all interstitial lung diseases are IPF.
Other examples of interstitial lung diseases include asbestosis, silicosis, nonspecific interstitial pneumonia, idiopathic interstitial pneumonias, hypersensitivity pneumonitis, and radiation pneumonitis. ILD is also associated with certain autoimmune diseases such as rheumatoid arthritis and certain connective tissue diseases like scleroderma and lupus.
What are the symptoms of ILD?
Common symptoms of interstitial lung diseases include dyspnea (shortness of breath) that worsens with exercise, a dry, hacking cough that does not produce phlegm, extreme tiredness, and weakness. Other symptoms may include discomfort in the chest, labored breathing (fast and shallow breathing), loss of appetite, and unexplained weight loss.
What are the risk factors for interstitial lung disease?
People who are at an increased risk of developing interstitial lung disease include those over the age of 70 years, people assigned male at birth, smokers, those who have had radiation therapy to the chest, and people with a history of lung conditions such as chronic obstructive pulmonary disease (COPD), pneumonia, and tuberculosis. In addition, those whose occupations expose them to inhaled irritants like asbestos, silica, dust, molds, bacteria, and fungi are also at an increased risk of developing interstitial lung diseases.
What are the four stages of interstitial lung disease?
Interstitial lung disease is a chronic progressive condition that typically gets worse with time with worsening lung scarring. The symptoms of ILD may not be noticeable until the disease has progressed to more advanced stages. As the disease progresses, however, most people with interstitial lung disease experience a gradual worsening of lung function. However, notably, the rate of progression of the condition can vary greatly from person to person. Therefore, unlike many other chronic diseases, there are no formally defined "stages" of interstitial lung disease. Everyone’s course is different. Nonetheless, doctors may use the following informal categories to describe the severity of a patient’s symptoms and their need for oxygen therapy:
- Stage 1: No need for oxygen.
- Stage 2: Need for oxygen with activity and acute exacerbations.
- Stage 3: Need for oxygen around the clock.
- Stage 4: Need for high-flow oxygen.
How are interstitial lungs diseases diagnosed?
Doctors use a variety of tests to diagnose lung problems, check lung function, and make an accurate diagnosis. If your healthcare provider suspects interstitial lung disease they may refer you to a respiratory medicine specialist. The specialist will perform a physical exam and may order blood tests, pulmonary function tests, peak flow monitoring, arterial blood gas, imaging studies to identify disease-related changes in your lungs, bronchoscopy, and lung biopsy or bronchoalveolar lavage.
How are interstitial lung diseases treated?
Treatment depends on the underlying cause and the severity of the interstitial lung disease. For example, in people with newly diagnosed interstitial lung disease with early symptoms such as mild shortness of breath, dry cough, and fatigue, treatment may consist of medications to slow down lung scarring or fibrosis and lifestyle modifications like quitting smoking and continued exercise. In contrast, those with more advanced interstitial lung disease may require oxygen therapy. People with end-stage interstitial lung disease may be candidates for a lung transplant.
As mentioned above, interstitial lung disease causes permanent lung damage. It is not usually possible to fix lung scarring that has already occurred. However, the following treatments can slow down the progression of the disease and improve symptoms:
- Corticosteroids such as prednisone help to reduce inflammation during an acute exacerbation (long-term use of these drugs carries several risks).
- Anti-fibrotic agents such as nintedanib (Ofev) and pirfenidone (Esbriet) slow down lung scarring. They are FDA-approved drugs for idiopathic pulmonary fibrosis, a common type of interstitial lung disease.
- Cytotoxic drugs like azathioprine, cyclophosphamide, and mycophenolate mofetil (Myfortic, Cellcept) slow down lung fibrosis by suppressing the immune system.
- Biologic agents like rituximab are used to treat autoimmune diseases associated with interstitial lung disease.
- Pulmonary rehabilitation (breathing exercises) helps to make the lungs stronger and improve oxygen and carbon dioxide exchange.
- Oxygen therapy as needed.
- Lung transplant for severe cases of interstitial lung disease.
What are the signs of the end stages of interstitial lung disease?
The following signs and symptoms may be present at the end stages of interstitial lung disease:
- Severe shortness of breath
- Difficulty breathing
- Need for high-flow oxygen
- Troublesome cough
- Chest discomfort
- Frequent acute exacerbations (flare-ups)
- Loss of appetite and weight loss
- Sleep disturbances
- Anxiety and depression
Note that each person’s course is different. The presence of these symptoms does not necessarily indicate that a person is close to death.
Which interstitial lung disease has the worst prognosis?
Severe interstitial lung disease has the worst prognosis (outlook). It can lead to life-threatening complications such as pulmonary hypertension (high blood pressure in the lungs), pneumothorax (collapsed lung), lung infections, respiratory failure, and lung cancer.
What is the life expectancy of a person with mild interstitial lung disease?
The life expectancy of a person with mild interstitial lung disease may be normal with minimal treatment or no treatment. The outlook tends to be particularly good for people with a stable disease that is not worsening over time. However, people with severe interstitial lung disease or rapidly worsening lung function may live for only 3-5 years after they have interstitial lung disease diagnosed.
How to prevent interstitial lung disease?
Sometimes interstitial lung disease is idiopathic (cause unknown), and there is nothing you can do to prevent it. However, certain precautions can lower your risk of ILD:
- Avoid exposure to toxic substances such as asbestos, silica, and harmful chemicals.
- Avoid exposure to substances that cause allergic reactions, like bird feathers and droppings, grains, hay, and HVAC systems.
- Wear a respirator if you are working around inhaled irritants.
- Manage autoimmune diseases by following your healthcare provider’s treatment recommendations.
- Quit smoking if you smoke.
References:
- https://www.lung.org/lung-health-diseases/lung-disease-lookup/interstitial-lung-disease
- https://my.clevelandclinic.org/health/diseases/17809-interstitial-lung-disease
- https://www.mayoclinic.org/diseases-conditions/interstitial-lung-disease/symptoms-causes/syc-20353108
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/interstitial-lung-disease-pulmonary-fibrosis
- https://www.lung.org/lung-health-diseases/lung-disease-lookup/pulmonary-fibrosis/patients/how-is-pulmonary-fibrosis-treated/medications#:










SOCIAL