Peripheral Artery Disease: Treatments & Prevention
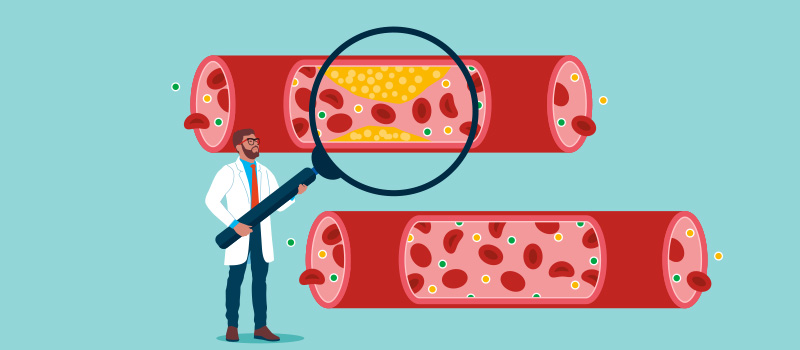
Peripheral artery disease (PAD) is a vascular disease in which there is reduced blood flow to the arms and legs due to the narrowing of the arteries. It occurs due to atherosclerosis (a buildup of fatty plaque) in the walls of the blood vessels. In addition, atherosclerosis also increases the risk of other serious health conditions and cardiovascular events such as heart attack and stroke.
There are several things you can do to prevent peripheral artery disease. Effective treatments are available if you develop this condition. Please continue reading to learn more.
What are the symptoms of peripheral arterial disease?
In people with peripheral artery disease, poor blood flow causes leg symptoms such as intermittent claudication (pain or cramps with walking or climbing stairs), aching and cramping in the arms when doing manual tasks, coldness, numbness, weakness, skin color changes, weak or absent pulse in the legs or feet, non-healing sores on the feet or legs, hair loss, and erectile dysfunction in men. When the disease is severe, PAD symptoms can include ischemic rest pain (leg pain at rest or when lying down).
What are the risk factors for peripheral artery disease?
Risk factors for peripheral arterial disease include high cholesterol, high blood pressure, high blood glucose, and high levels of homocysteine (an amino acid linked to coronary artery disease). Other risk factors are obesity, age above 65 years, and a family history of heart disease, stroke, or peripheral artery disease.
Without proper diagnosis and treatment, peripheral artery disease can cause serious complications such as critical limb ischemia and tissue death, requiring limb amputation in severe cases.
How do doctors diagnose PAD?
Doctors can make a diagnosis of peripheral artery disease based on the results of blood tests (cholesterol, blood sugar levels), ankle-brachial index (a test that compares blood pressure in the ankle and arm), Doppler ultrasound imaging to identify blocked arteries, and computed tomography or magnetic resonance angiography where a dye is used to show a blocked artery more clearly.
What is the initial treatment for peripheral artery disease?
The initial treatment for peripheral artery disease includes the following. Incidentally, these measures are also good for heart health.
Engage in exercise programs
Regular physical activity improves PAD symptoms by helping the body use oxygen more efficiently. Your healthcare provider may recommend a supervised exercise program to gradually increase your pain-free walking distance. The supervised exercise training may be painful initially. But if you stick with the supervised exercise therapy, over time, you'll be able to walk longer distances and climb stairs without pain. If you have severe pain, it may help to sleep with the head of your bed slightly raised so that your legs are below heart level.
Eat a balanced diet
Foods high in saturated fat increase your risk of developing fatty plaques in the blood vessels. A healthy diet is, therefore, an important part of PAD treatment. Your healthcare professional will advise you to limit the intake of saturated fats, salt, and sugar and to eat more fruits, vegetables, whole grains, nuts, seeds, healthy fats, and lean meats.
Quit smoking
Smoking intensifies the problems caused by the buildup of plaque in your blood vessels. The nicotine in tobacco causes narrowing of the blood vessels and can cause severe symptoms of peripheral artery disease. Your healthcare provider will recommend quitting smoking to help restore blood flow.
What precautions should I take if I have peripheral artery disease?
In addition to the lifestyle changes described above, it is important to take good care of your feet if you have a diagnosis of peripheral artery disease (PAD), especially if you also have diabetes, because you are at risk of developing poorly healing or non-healing sores and ulcers on your lower legs and feet due to the poor blood flow.
-
Keep your feet clean, dry, and well moisturized.
-
Wear well-fitting shoes.
-
Treat fungal infections such as athlete's foot promptly.
-
Be careful when trimming toenails.
-
Inspect your feet daily for sores or injuries and get prompt care if you notice any.
-
See a podiatrist (foot doctor) for corns, calluses, or bunions.
What medications are prescribed for peripheral artery disease?
Some of the medications used to treat PAD include:
-
Cholesterol-lowering drugs such as statins to reduce the buildup of atherosclerotic plaque in the artery wall.
-
Antihypertensive drugs to control high blood pressure which can make blood flow slower.
-
Antidiabetic drugs to control blood sugar levels.
-
Antiplatelet therapy with aspirin or clopidogrel (Plavix) to prevent blood clots and ensure blood moves easily.
-
Medications to treat peripheral artery disease such as cilostazol or pentoxifylline. These drugs work by thinning the blood and widening the blood vessels, thereby increasing blood flow to the limbs and controlling intermittent claudication (leg pain).
What are the surgical procedures for peripheral artery disease?
If you have severe peripheral artery disease, your healthcare provider may refer you to a vascular specialist who may recommend surgical endovascular therapies such as:
-
Thrombolytic therapy to dissolve a blood clot that may be blocking an artery. The clot-dissolving drug can be placed directly in the artery.
-
Balloon angioplasty and stent placement to open blocked arteries. This procedure is done by guiding a catheter (a thin, flexible tube) into the narrowed blood vessel and inflating a tiny balloon to widen the artery and improve blood flow. A stent (a small tube made of wire mesh) may be left in place to keep the artery open.
-
Atherectomy to remove plaque buildup from an artery. This endovascular intervention is also done with a catheter, similar to an angioplasty.
-
Bypass surgery to create a bypass (re-routing) around the blocked artery. This is done using either a healthy blood vessel from some other part of the body or a synthetic blood vessel.
Can peripheral artery disease be prevented?
Yes, peripheral artery disease can be prevented by eating a healthy diet, getting regular exercise, quitting smoking, maintaining a healthy weight, and controlling blood pressure, blood sugar, and blood cholesterol levels. These measures will not only help to prevent peripheral artery disease but also lower your risk of serious health problems such as heart attack and stroke.
How can I improve my peripheral artery circulation?
You can improve your peripheral artery circulation by quitting smoking, choosing a heart-healthy diet, getting regular physical exercise, and maintaining a healthy body weight. These measures will improve your ability to walk, climb stairs, perform routine daily activities, and improve your overall quality of life. They will also lower your risk of needing a leg amputation due to severe peripheral artery disease.
What is the best vitamin for peripheral artery disease?
Some of the vitamins and dietary supplements that may benefit people with peripheral artery disease include omega-3 fatty acids, folate and B vitamins, vitamin D, and vitamin E. However, there is no strong scientific evidence that these supplements can reduce the risk of developing peripheral artery disease or stop it from getting worse. Some supplements carry an increased risk of complications such as bleeding. Always check with your healthcare provider before taking any over-the-counter dietary supplements for peripheral artery disease.
References:









SOCIAL