What’s the Buzz
The Bee Healthy Blog
Why Your BMI is an Outdated Way to Measure Health
Body mass index (BMI) is a popular method to measure obesity and evaluate health. Health professionals and the general public have been using it for decades as a health assessment tool based on body size. However, more recently, BMI has been criticized for being an oversimplified measure of health risk.
Please continue reading to find out why body mass index (BMI) may be an outdated and inaccurate calculation. Also, learn what you should use instead of BMI to assess your health risks.
What is body mass index (BMI)?
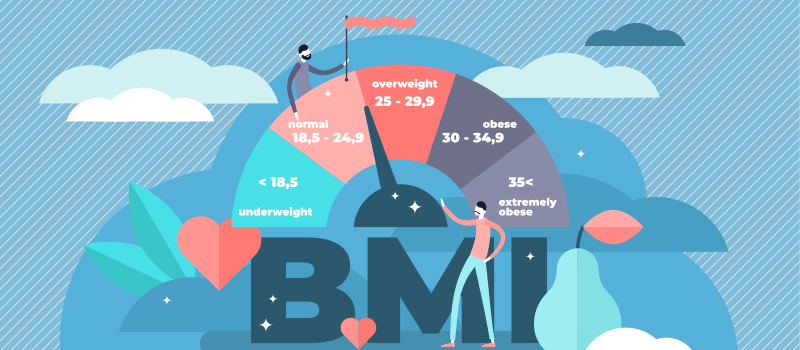
Body mass index or BMI is a number that takes into account your height and weight to arrive at a rough estimation of your health status. BMI is obtained by dividing your weight in kilograms by your height in meters squared (kg/m2). A BMI result between 18.5 and 25 is considered normal. Here are the categories of BMI results:
| BMI less than 18.5 | Underweight |
| BMI between 18.5 and 24.9 | Normal |
| BMI between 25 and 29.9 | Overweight |
| BMI over 30 | Obese |
According to the World Health Organization, over 3 million people worldwide are overweight or obese based on BMI. BMI is commonly used as a screening number to assess weight and health risks for conditions like diabetes, high blood pressure, high cholesterol, heart disease, sleep apnea, and certain types of cancer. Yet, BMI, which was originally developed more than 100 years ago and evolved to its current avatar in the 1940s, could well be an outdated measure of health risks.
Is BMI a good way to measure a person's health?
Body mass index is by no means a perfect test. For instance, BMI results could be meaningless in a pregnant woman or a person with very high muscle mass. It also is not a good tool to assess health risks in very young children or elderly individuals.
But BMI is not completely irrelevant. Generally speaking, a BMI in the overweight or obese category indicates an increased risk of developing a variety of health conditions linked to excess body weight. Therefore, BMI remains a quick, easy, and affordable way to assess a person’s health risk.
Is BMI an outdated measure?
There are a few different reasons why the BMI scale may not be the best way to screen for a person's health status.
Body fat percentage
Body fat percentage is a calculation of a person’s body fat stored compared to their total body weight. A person’s body fat percentage can be accurately measured with DXA, which is a type of X-ray machine used to measure bone mass or bone density. You can also estimate body fat percentage using bioelectrical impedance or skin fold calipers.
The advantage of body fat percentage over BMI is it takes into account a person’s body composition, i.e., what percent body fat and what percent muscle mass they have. Muscle tissue has more density than fat and muscle weighs more than fat. Therefore, some people with more muscle mass, such as weightlifters and athletes, may be considered overweight on the basis of BMI. In such individuals, BMI can indicate excess weight, a greater risk of health conditions, and an increased mortality risk, despite the person’s peak physical condition.
Body fat percentage is a better measure of a person’s health risk because a higher health risk is related to excess body fat and not excess body weight.
Body fat distribution
Health professionals say that the location of body fat is an important factor when evaluating increased health risks. In general, upper body fat, abdominal fat, and visceral fat correlate to health problems more than fat in other parts of the body. (Visceral fat is fat stored around the abdominal organs like the intestines, liver, and pancreas).
The BMI scale does not measure body fat or take into account fat distribution when assigning a higher risk to people with excess body weight. Indeed, studies have shown that it is not a person’s weight or even the amount of body fat stored but where the fat is stored that determines the risk of diabetes, heart attack, stroke, and other serious health complications.
In other words, a person with a normal BMI but a high waist-to-height ratio could be at high risk of heart disease due to more body fat stored around vital organs. Two people with the same BMI can have very different risk profiles for cardiovascular disease based on their waist circumference or waist-to-hip ratio.
Therefore, a large waist circumference or fat in the midsection is considered a better indicator of the high risk of health problems rather than a simplified height and weight tool like BMI.
Demographics
When BMI was originally created, it was based on a European Anglo-Saxon population. Many health professionals now believe that measuring BMI is not an accurate way of assessing disease risk for other ethnic groups.
For instance, research suggests that Asians could have double the risk of developing type 2 diabetes as Caucasians with the same BMI. In other words, a high disease risk can start at a lower BMI and waist circumference in Asian populations compared to Caucasians.
Studies have also shown that a higher BMI may in fact be healthy in Black women than is indicated by the standardized BMI scale. For White and Hispanic women, on the other hand, a lower BMI may be considered healthy. Therefore, when measuring risk factors for diabetes, a BMI of 33 in Black women and a BMI of 29 in White women could be a more accurate cut-off number.
These findings suggest that the BMI scale needs to be personalized to define obesity and calculate disease risk more accurately in different demographics.
What to use instead of BMI?
BMI is not completely outdated. It continues to be an inexpensive and easy way to assess whether you are a normal weight, need to lose weight, or gain weight to stay healthy. Many studies have shown that a person’s risk of chronic disease is higher with a BMI over 30 or under 18.5.
With that said, there are other predictors of health risk available that are more accurate. Experts at the Harvard Medical School list five metabolic factors that increase a person’s risk of diabetes, stroke, heart disease, and other chronic diseases:
- High blood cholesterol: A total cholesterol level above 239 mg/dL is linked to a higher risk of chronic health conditions.
- High triglycerides: A triglyceride level above 200 mg/L is associated with a higher risk of chronic disease.
- High blood sugar: A blood sugar level above 125 mg/dL is linked to a greater risk of chronic disease.
- High blood pressure: Blood pressure numbers over 140/90 mmHg are a health risk.
- Waist circumference: Excess fat in the midsection with a waist circumference of 35 inches or more in women and 40 inches or more in men is linked to an increased health risk.
BMI is clearly not a perfect measure for defining obesity or identifying an increased risk of health conditions. But it can still be a useful starting point. It is a good idea to keep an eye on your body mass index as a measure of body weight, but at the same time to recognize its limitations and turn to your doctor for health advice.
References:
- https://www.health.harvard.edu/blog/how-useful-is-the-body-mass-index-bmi-201603309339
- https://www.sciencedaily.com/releases/2017/11/171128091015.htm#
- https://www.hsph.harvard.edu/obesity-prevention-source/ethnic-differences-in-bmi-and-disease-risk/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6818706/

SOCIAL