What’s the Buzz
The Bee Healthy Blog
Medication & Supplement Guidelines After Bariatric Surgery

Obesity is the leading cause of many chronic metabolic diseases and cardiovascular diseases, such as high blood pressure, nonalcoholic fatty liver disease, high cholesterol, and type 2 diabetes, to name a few. Bariatric surgery (weight loss surgery) can help obese patients who meet specific criteria to live healthier and longer lives by reducing the mortality risk of the weight-related health problems mentioned above.
Just like any procedure, there are risks associated with bariatric surgery. Along with health complications associated with the surgery, like infections and bleeding, there are long-term risks such as bowel obstruction, low blood sugar, and malnutrition.
Problems with absorbing certain nutrition and other restrictions with medications are one of the challenges people face post-surgery. For example, people who have undergone bariatric procedures develop nutritional deficiencies, necessitating the use of dietary supplements. Also, people who have undergone bariatric surgery may need to take certain prescription medications and avoid other drugs. Additionally, many patients are able to discontinue certain medications as their obesity-related health issues improve after bariatric surgery. Unlike other complications, malnutrition and other medication-related problems can be managed largely by promoting patients’ education.
Being knowledgeable about the type of supplements along with the do’s and don’t’s helps patients to feel more empowered in their weight loss journey. If you or your loved one are interested or have undergone bariatric surgery, please continue reading to learn more about the guidelines for medications and supplements after bariatric surgery.
Am I a candidate for bariatric surgery?
Bariatric surgery can be considered after lifestyle changes with diet and exercise were attempted but unable to yield adequate weight loss. You may be a candidate for bariatric surgery if you meet the following criteria:
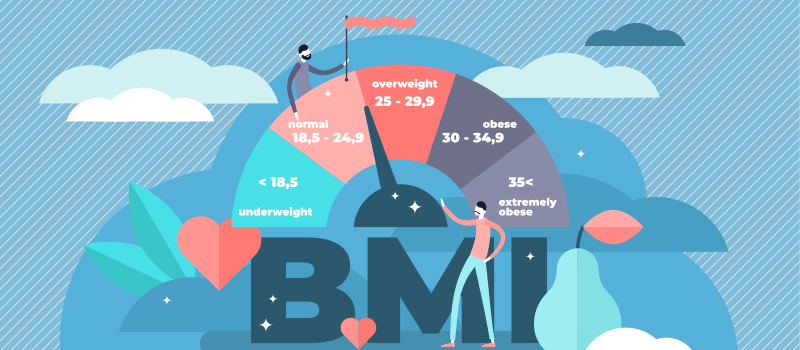
- You have a body mass index (BMI) of 40 or higher, which is classified as class III obesity (formerly referred to as morbid obesity).
- You have a BMI between 35 and 39.9 and a weight-related medical condition such as high blood pressure, uncontrolled sleep apnea, or type 2 diabetes.
- You have a BMI between 30 and 34 and a serious weight-related medical condition.
What are the different types of bariatric surgery?
Weight loss surgery is categorized into 3 types. Your surgeon and primary care team will help you determine the type that is right for you depending on your health history, weight loss goals, and personal preference. Below are the three types:
- Restrictive: limits your food intake by reducing the size of your stomach
- Malabsorptive: reduces the food absorption by bypassing (go around or go past) parts of the small intestine
- Combination: restrictive and malabsorptive
Gastric restrictive procedures include laparoscopic adjustable gastric banding (LABG) and laparoscopic sleeve gastrectomy. These bariatric surgeries limit the amount of food you can eat but leave the normal digestive process intact.
Biliopancreatic diversion gastric bypass is a complicated procedure removing part of the stomach and bypasses most of the intestine; it is reserved for those with a BMI greater than 50. This procedure is mainly malabsorptive.
A laparoscopic Roux en Y gastric bypass is a combined restrictive and malabsorptive procedure in which the surgeon creates a small pouch from the stomach and connects it to the small intestine.
Why is medication management necessary for bariatric surgery patients?
A bariatric surgery patient needs to take certain medications and supplements to avoid medical and nutritional complications. Here are some reasons why clinical practice guidelines for medications have been developed for bariatric patients:
- Macronutrient and micronutrient deficiencies are common after bariatric surgery. These nutrient and vitamin deficiencies need to be corrected with adequate supplementation. For example, reduced iron absorption can lead to a micronutrient deficiency of iron. Vitamin D deficiency may require postoperative alterations in supplements.
- Rapid weight loss after bariatric surgery can increase the risk of certain conditions like cholelithiasis (gallstones) and nephrolithiasis (kidney stones). Medications and lifestyle changes can help lower these risks.
- Bone resorption increases after bariatric surgery, leading to low bone mineral density. Calcium and vitamin D supplementation are necessary to lower fracture risk.
- Bariatric patients can develop problems such as dumping syndrome due to changes in gastrointestinal physiology. This condition is associated with rapid emptying of food from the stomach into the intestines. Anti-diarrheal drugs may need to be prescribed to prevent this from occurring.
- The dramatic physiologic changes after bariatric surgery frequently allow bariatric patients to reduce or come off treatments for chronic metabolic diseases. Medication adjustments may need to be made for drugs used to treat high blood pressure, type 2 diabetes, and high cholesterol due to improvement in these conditions.
- Bariatric surgery is not a cure for obesity. It is a tool that aids rapid weight loss, prevents weight regain, and helps people adhere to a healthy lifestyle. Medication management after bariatric surgery also includes avoiding medications that can cause weight gain and prescribing weight-loss medications, if needed.
What medications do you need after Roux en Y gastric bypass?
You will need to take some medications for the short term and some for the long term after a bariatric procedure. These include:
- A proton pump inhibitor such as omeprazole for about 6 months after bariatric surgery. This medication will lower your risk of stomach and intestinal ulcers due to excess gastric acid.
- A gallstone-dissolving medicine like ursodiol for about 6 months after gastric bypass surgery. This medication will reduce your risk of developing gallstones due to rapid weight loss in the postoperative period.
- An anti-diarrheal drug like octreotide to treat dumping syndrome if it does not get better with changes in diet. This medication is given by injection under the skin and slows the emptying of food from the stomach.
Can I take weight loss medication if I gain weight after weight loss surgery?
It is unknown why certain people lose and maintain 50% of their body weight while others regain all their lost weight. Some possibilities include genetics and the use of medications that promote weight gain before bariatric surgery, such as corticosteroids, antipsychotics, beta-blockers, and HIV medicines.
In addition to supporting patients’ adherence to diets and consistent exercise, there are studies regarding the use of medication to aid weight loss after bariatric surgery. The medications in these observational studies include FDA-approved weight loss medications such as phentermine, liraglutide, and off-label use of medications with potential weight-lowering effects such as metformin, topiramate, and canagliflozin.
There is no doubt about the importance of medications in therapy used post-bariatric surgery to aid with weight loss. However, the size of these observational studies are very small, and medications were used in weight regain rather than weight loss plateau (when the weight loss remains stagnant after surgery despite diets and exercise). More research is necessary to optimize the use of medication for weight loss after surgery and to learn about the type of medications in addition to the timing to initiate medication management.
Currently, the use of weight loss medication is case by case, based on the individual. Medical history and a gastrointestinal study are thoroughly evaluated prior to initiating medication to aid weight loss in patients after bariatric surgery.
When can you take regular vitamins after bariatric surgery?
You cannot take regular vitamins after bariatric surgery. Bariatric patients need to take bariatric-specific multivitamins indefinitely to compensate for nutrient deficiencies (vitamin and mineral deficiencies). This is because bariatric patients are at an increased risk of nutritional deficiencies. They have reduced nutrient absorption from the digestive tract and need to supplement nutrients obtained from food intake with special high-dose multivitamins.
What supplements do you need after bariatric surgery?
You need to take bariatric-specific multivitamins that contain high doses of all the necessary water-soluble vitamins like vitamin C, folic acid, and B vitamins; fat-soluble vitamins like vitamin A, D, E, and K; iron supplementation; and other mineral supplements.
Your doctor will also ask you to take a calcium supplement that contains 1,000 to 1,500 mg of calcium to address any calcium deficiency. The supplement is usually taken in 2-3 divided doses along with vitamin D to enhance calcium absorption. Calcium citrate is the preferred form over calcium carbonate.
Can bariatric surgery patients take regular medications?
Bariatric surgery patients can take capsules, chewable tablets, and liquid medications soon after their procedure. However, medications in tablet form need to be crushed for the first 3 months to prevent them from getting stuck in the gastrointestinal (GI) tract or not being absorbed properly. Your doctor or pharmacist will recommend alternatives for extended-release tablets which cannot be crushed.
When can I resume my usual medications after gastric bypass surgery?
Your doctor will give you detailed instructions on resuming your usual medicines for other health conditions after bariatric surgery. It’s important to keep all your healthcare appointments during this time because rapid weight loss may necessitate frequent medication adjustments.
Women of childbearing age will need to use an intrauterine device (IUD) for effective birth control in the first 12-18 months after bariatric surgery. Doctors do not recommend getting pregnant in the first year after bariatric surgery because the rapid weight loss and reduced food intake impact nutritional status and can compromise the health of the baby, resulting in birth defects.
What medications to avoid after metabolic and bariatric surgery?
Your bariatric surgery team will tell you to avoid non-steroidal anti-inflammatory drugs (NSAIDs) indefinitely. These drugs increase the risk of stomach ulcers. Examples include aspirin, ibuprofen (Motrin, Advil), naproxen (Aleve), and celecoxib (Celebrex). People who have undergone a sleeve gastrectomy might be able to take these medications about 3 months after the surgery once the sleeve has healed.
Which medications should bariatric patients stop after surgery?
Gastric bypass surgery can lead to a significant amount of weight loss, in turn, reducing the risks of chronic metabolic health conditions while improving overall health. This allows many patients who have undergone bariatric surgery to lower the dose of or even discontinue medications used to treat obesity-related conditions such as type 2 diabetes and hypertension. Close postoperative monitoring and medical management are necessary by the primary care provider, clinical endocrinologists, and bariatric team to ensure that all medications are optimized following bariatric surgery.
References:
- https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=85&contentid=P07861#
- https://www.ucsfhealth.org/education/life-after-bariatric-surgery
- https://www.ncbi.nlm.nih.gov/books/NBK481901/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6114136/
- https://www.uspharmacist.com/article/implications-of-bariatric-surgery-on-absorption-of-nutrients-and-medications
- https://www.mayoclinic.org/diseases-conditions/dumping-syndrome/diagnosis-treatment/drc-20371922#
- https://stanfordhealthcare.org/medical-treatments/g/gastric-bypass-surgery/types.html
- https://pubmed.ncbi.nlm.nih.gov/30779535/
- https://advances.massgeneral.org/digestive-health/journal.aspx?id=1297











SOCIAL